What is a Tumer? Understanding the Medical Terminology
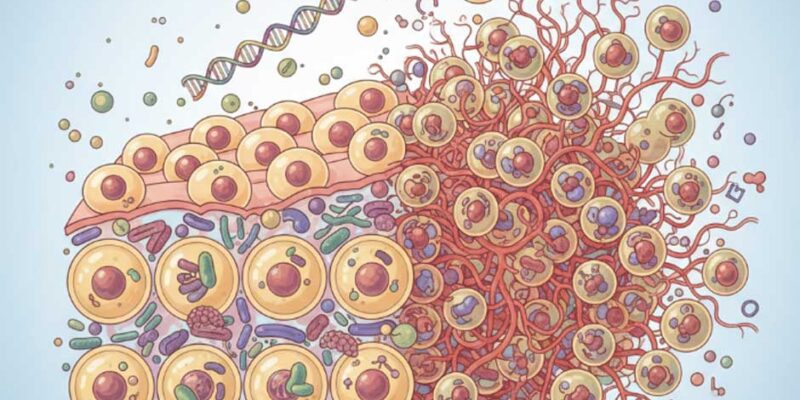
If you’ve come across the term “tumer,” you’re likely looking for information about “tumor” – a common misspelling that many people make when searching for medical information online. A tumor represents an abnormal mass of tissue that develops when our body’s cellular machinery goes awry.
Think of it this way: our bodies are constantly creating new cells to replace old, damaged ones. Sometimes, however, this process gets disrupted. Cells begin growing and multiplying faster than they should, or they simply refuse to die off when their time is up. The result? An unwanted collection of cells that we call a tumor.
These growths can appear virtually anywhere in the human body – from the obvious places like skin and muscles to hidden locations within our organs, bones, and glands. Recognizing what tumors are and how they behave is crucial for anyone wanting to understand this important health topic.
The Three Main Types of Tumors You Should Know
When doctors talk about tumors, they’re essentially discussing three distinct categories that behave very differently from one another. Understanding these differences can help you make sense of medical conversations and treatment decisions.
Benign tumors are the “good guys” in this story. While nobody wants any kind of abnormal growth, benign tumors stay put where they started. They don’t invade neighboring tissues or pack their bags to travel elsewhere in your body. Most of the time, they’re not life-threatening, though they can still cause problems if they decide to set up shop next to something important like your brain or heart.
On the opposite end of the spectrum, we have malignant tumors – the ones that earn the label “cancerous.” These are the troublemakers that can break through tissue boundaries and establish colonies in distant parts of your body through a process called metastasis. They’re the reason cancer can be such a serious diagnosis.
Then there’s the middle ground: premalignant tumors. Think of these as cells that are sitting on the fence. They haven’t crossed over into cancer territory yet, but they’re showing signs that they might. With proper monitoring and sometimes treatment, doctors can often prevent these fence-sitters from making the leap to malignancy.
Common Causes and Risk Factors Behind Tumor Development
The million-dollar question that most people ask is: “Why do tumors happen?” The honest answer is that it’s rarely just one thing. Tumor development is more like a perfect storm where multiple factors come together at the wrong time and place.
Your genes play a significant role in this story. Some people inherit genetic variations that make them more susceptible to developing certain types of tumors. If cancer runs in your family, you might have heard doctors mention terms like BRCA genes or Lynch syndrome. These aren’t guarantees that you’ll develop cancer, but they do mean you might need to be more vigilant about screening and prevention.
Then there’s the world around us. Our modern lifestyle exposes us to various substances that can damage our DNA over time. Tobacco smoke remains the heavyweight champion of cancer-causing agents, but it’s not alone. Chemical exposures at work, too much sun without protection, excessive alcohol consumption, and even some viral infections like HPV can all contribute to the problem.
What’s particularly interesting is how these factors can work together. Someone with a genetic predisposition might never develop cancer if they avoid environmental triggers. Conversely, someone with “good genes” might still face problems if they’re exposed to enough harmful substances over time.
Recognizing Tumor Symptoms: When to Seek Medical Attention
Here’s something that catches many people off guard: tumors don’t always announce their presence with obvious symptoms. Some can grow quietly for months or even years before causing any noticeable problems. Others might make themselves known relatively early in the process.
The tricky part is that many tumor symptoms can mimic other, less serious conditions. Persistent fatigue might just mean you’re working too hard, but it could also signal something more concerning. Unexplained weight loss might seem like a blessing if you’ve been trying to shed pounds, but losing weight without trying is actually a red flag that deserves medical attention.
Pay attention to your body’s signals. A new lump that you can feel under your skin, changes in existing moles, persistent cough that won’t go away, or unusual bleeding should all prompt a conversation with your healthcare provider. The key word here is “persistent” – symptoms that stick around for weeks rather than days.
Remember, most of these symptoms turn out to be something benign. But the peace of mind that comes from getting checked out is worth the temporary anxiety of not knowing. Early detection remains one of our most powerful tools in fighting cancer, so don’t hesitate to speak up when something doesn’t feel right.
Modern Diagnosis Methods for Tumor Detection
When your doctor suspects a tumor, they have an impressive arsenal of diagnostic tools at their disposal. The goal is to answer three critical questions: Is it really a tumor? If so, what type is it? And has it spread anywhere else?
The gold standard for tumor diagnosis remains the biopsy. This involves taking a small sample of the suspicious tissue and having a pathologist examine it under a microscope. While the word “biopsy” might sound scary, many can be done as outpatient procedures with minimal discomfort. The pathologist acts like a detective, looking for specific cellular characteristics that reveal whether the tumor is benign or malignant.
Modern imaging technology has revolutionized how doctors visualize tumors inside the body. CT scans provide detailed cross-sectional images, while MRIs offer exceptional soft tissue contrast. PET scans can actually show metabolic activity, helping doctors distinguish between active tumor tissue and scar tissue from previous treatments.
Blood tests add another layer of information. Certain tumors release specific proteins called tumor markers into the bloodstream. While these markers aren’t perfect diagnostic tools on their own, they can provide valuable clues and help monitor treatment progress over time.
Treatment Approaches: From Surgery to Advanced Therapies
The landscape of tumor treatment has evolved dramatically over the past few decades. What once might have been a one-size-fits-all approach has transformed into highly personalized treatment plans that consider not just the tumor itself, but also the individual patient’s overall health, preferences, and life circumstances.
Surgery remains a cornerstone of tumor treatment, especially when the growth is localized and accessible. The surgeon’s goal is typically to remove the entire tumor along with a margin of healthy tissue to ensure no abnormal cells are left behind. For benign tumors, surgery might be the only treatment needed. For malignant tumors, surgery often serves as the opening act in a more comprehensive treatment plan.
Radiation therapy uses precisely targeted high-energy beams to damage cancer cells’ DNA, preventing them from reproducing. Modern radiation techniques can focus these beams with remarkable accuracy, minimizing damage to surrounding healthy tissue. Chemotherapy, on the other hand, uses powerful drugs that travel throughout the body to seek and destroy cancer cells wherever they might be hiding.
The newest players in the treatment game are immunotherapy and targeted therapy. Immunotherapy essentially teaches your immune system to recognize and attack cancer cells more effectively. Targeted therapy uses drugs designed to interfere with specific molecular pathways that cancer cells depend on for survival. These approaches often cause fewer side effects than traditional chemotherapy because they’re more selective in their targets.
Prevention Strategies and Lifestyle Modifications
While we can’t control our genes or completely eliminate all cancer risks from our environment, there’s actually quite a bit we can do to stack the odds in our favor. The encouraging news is that many of the lifestyle choices that reduce cancer risk also happen to improve overall health and quality of life.
The foundation of cancer prevention starts with the basics that your grandmother probably told you: eat your vegetables, stay active, and don’t smoke. A diet rich in colorful fruits and vegetables provides antioxidants that help protect our cells from damage. Regular physical activity not only helps maintain a healthy weight but also boosts immune function and helps regulate hormones that can influence cancer risk.
Tobacco avoidance deserves special mention because it’s the single most preventable cause of cancer. If you currently smoke, quitting is the best gift you can give your future self. If you don’t smoke, avoiding secondhand smoke is equally important. Alcohol moderation is another key factor – while an occasional drink might be fine for most people, regular heavy drinking significantly increases cancer risk.
Don’t underestimate the power of regular medical check-ups and age-appropriate cancer screenings. These visits can catch problems early when they’re most treatable. Mammograms, colonoscopies, Pap smears, and other screening tests have saved countless lives by detecting cancers before symptoms appear.
Living with Tumors: Prognosis and Quality of Life
Receiving a tumor diagnosis can feel overwhelming, but it’s important to remember that outcomes vary tremendously depending on many factors. The type of tumor, how early it’s caught, your overall health, and how well you respond to treatment all play crucial roles in determining your prognosis.
For people with benign tumors, the news is generally very good. Most benign tumors can be successfully treated or managed without significantly impacting life expectancy or quality of life. Even when surgery is required, recovery is typically straightforward, and the problem is often solved permanently.
The picture for malignant tumors is more complex, but there’s reason for optimism. Cancer survival rates have improved dramatically over the past several decades thanks to earlier detection, better treatments, and more personalized approaches to care. Many people with cancer go on to live full, productive lives, and some are cured completely.
Living with a cancer diagnosis involves more than just medical treatment. Support systems play a crucial role in helping people navigate this challenging journey. This might include family and friends, support groups, counseling services, and healthcare teams that specialize in helping people maintain the best possible quality of life throughout treatment and beyond.
Follow-up care is an essential part of the long-term picture. Regular monitoring helps ensure that any changes are caught early, and many people find that these check-ups become routine parts of their lives rather than sources of anxiety. The goal is always to help people live as normally as possible while staying vigilant about their health.